AI FOR HEALTHCARE PAYERS
Healthcare AI agents your members can trust
From benefits education and claims support to enrollment and care navigation, our AI Agents deliver secure, personalized, and consistent experiences that help members get answers faster.

Here’s how healthcare payers use Nexora
24/7 member support
Automate high-volume member inquiries with secure, compliant, and easy-to-integrate AI agents that help members understand their coverage, benefits, and next steps—anytime.
- Benefits explanations
- Claims status inquiries
- Eligibility and coverage checks
- General member FAQs
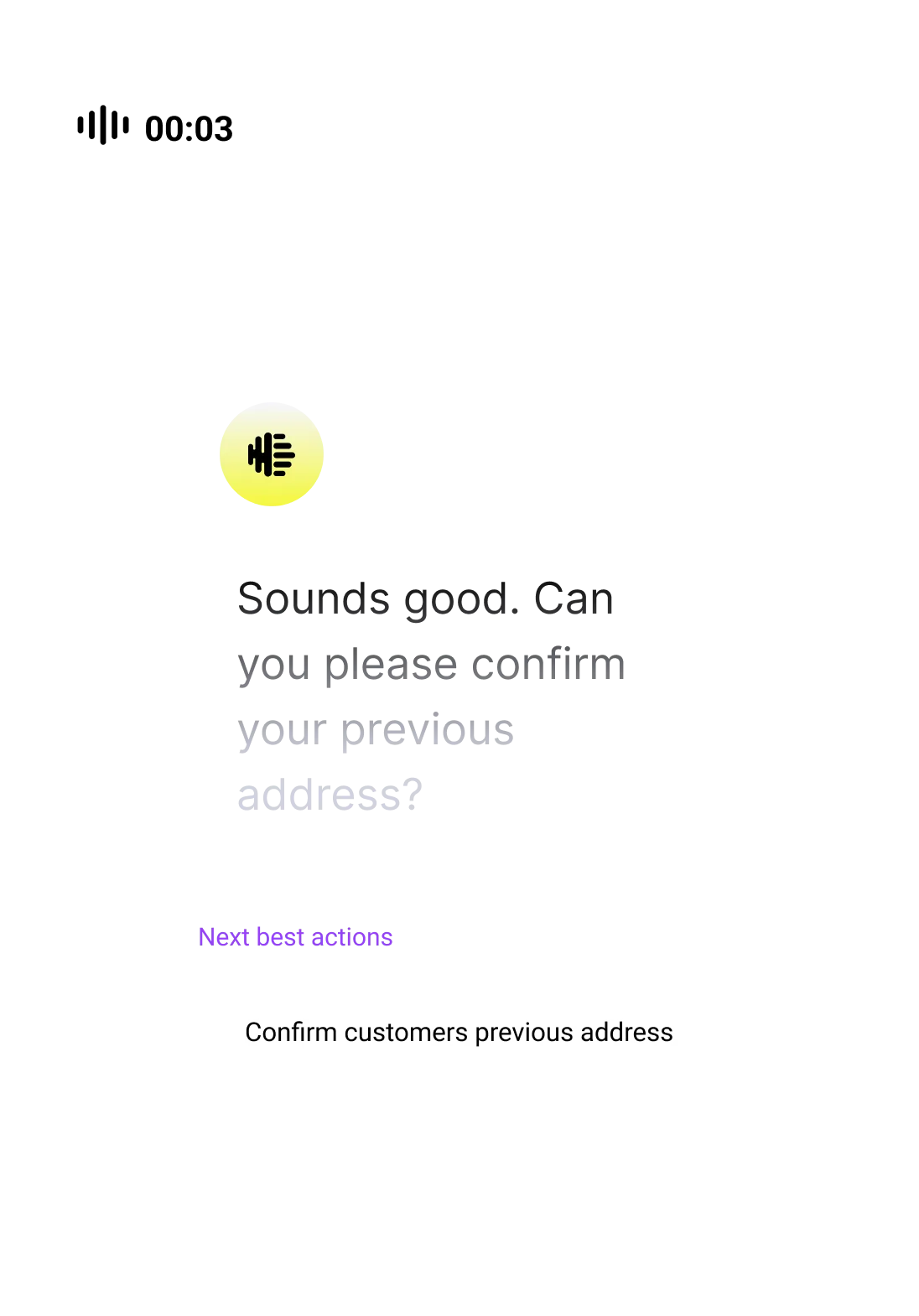
Copilot for payer teams
Enable service representatives and operations teams with an AI Copilot that delivers real-time guidance, policy context, and recommended actions during member interactions.
- Policy and plan guidance
- Escalation recommendations
- Claims resolution support
- Member outreach assistance
Cost and service visibility
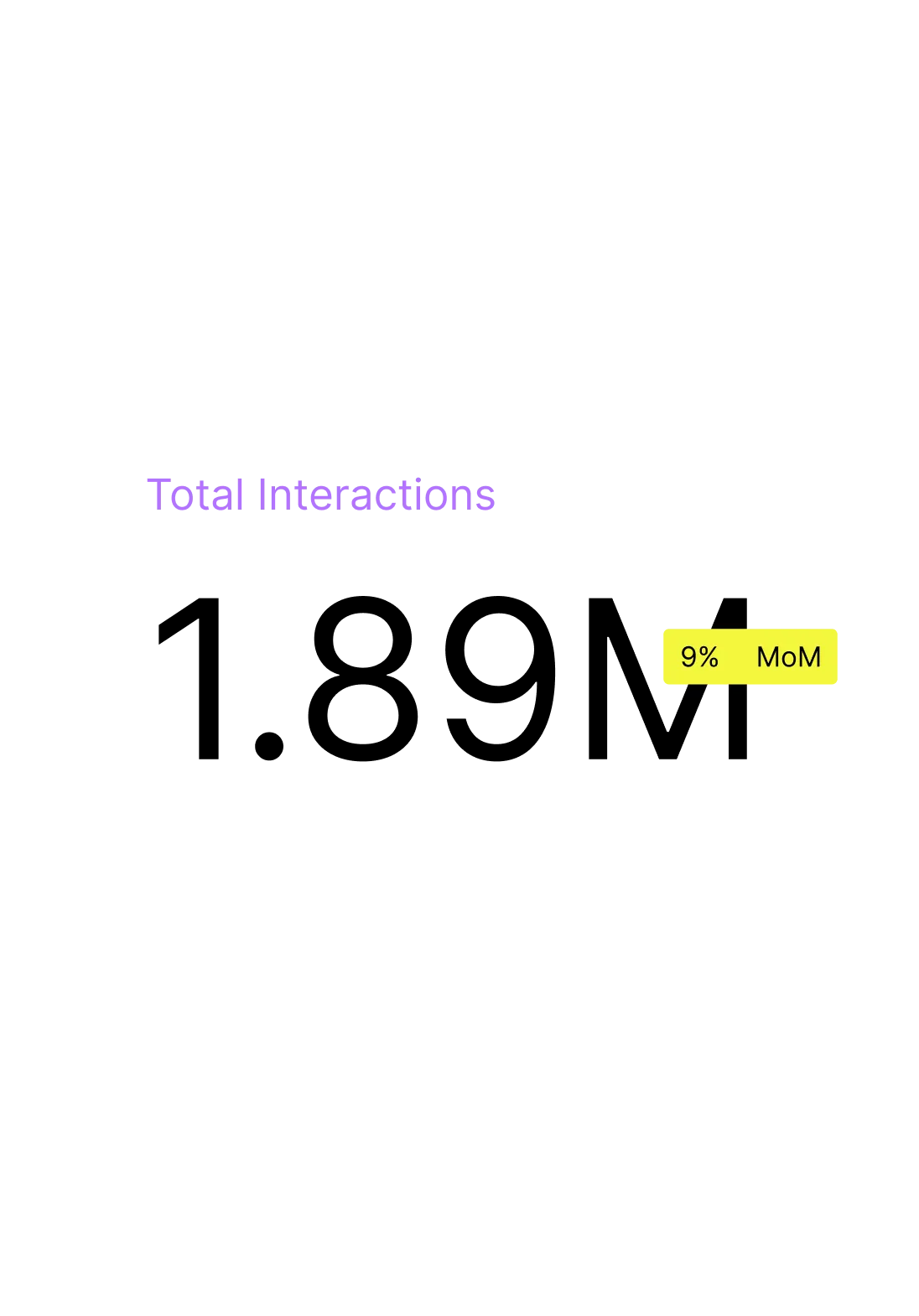
Analyze 100% of member interactions to identify cost drivers, improve service efficiency, and make data-driven decisions that enhance member satisfaction.
- Call and inquiry drivers
- Claims friction points
- Coverage confusion trends
- Process improvement insights
Seamless integration with payer systems
Connect your AI Agents to the platforms your teams already use
View all integrations




Why healthcare payers choose Nexora
01
01
Trusted Partner
We partner with healthcare payers to modernize member service operations, helping teams address immediate efficiency challenges while improving long-term member trust and satisfaction.
02
02
Agentic Architecture
Design AI agents using natural language prompts that reflect your plans, policies, and workflows. Agents integrate with payer systems to take informed, compliant action.
03
03
AI Agent Trust
Built for regulated healthcare environments, Nexora applies rigorous monitoring and quality controls to ensure AI Agent interactions meet compliance, accuracy, and privacy standards.
04
04
Continuous Learning Loop
By learning from real member interactions and simulations, AI Agents continuously improve—helping payer organizations adapt to changing policies and member needs.
Real results from actual customers
Ready to invest?
Our AI Agents help healthcare payers improve member experiences across benefits, claims, enrollment, care navigation, and ongoing support.
FAQ
Nexora helps healthcare payers automate high-volume member interactions, improve service efficiency, and reduce operational costs. AI Agents assist with benefits questions, claims status, eligibility checks, and general member support.